Diseases & Conditions
Dupuytren's Disease
Dupuytren's disease is a condition that affects the palmar fascia — the fibrous layer of tissue that lies underneath the skin and above the tendons, nerves, blood vessels, and bones in the palm and fingers.
In patients with Dupuytren's, the fascia thickens and contracts (shortens) over time. The fascia may pull on the fingers during this process, causing them to be forced inward, toward the palm. This may make it difficult or impossible to fully straighten the fingers, resulting in what is known as a "Dupuytren's contracture."
In some people, a worsening Dupuytren's contracture can interfere with hand function, making it difficult to perform daily activities. When this occurs, there are nonsurgical and surgical treatment options available to help slow the progression (worsening) of the disease and improve motion in the affected fingers.
Description
The fascia is a layer of tissue that helps to anchor and stabilize the skin on the palm side of the hand. Without the fascia, the skin on your palm would be as loose and moveable as the skin on the back of your hand. In patients with Dupuytren's disease, this palmar fascia gradually thickens and contracts (shortens).
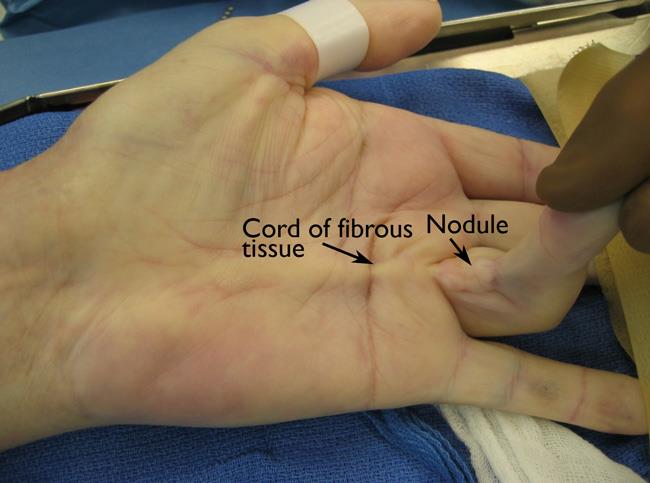
Dupuytren's is usually first detected when lumps of tissue, or nodules, form under the skin in the palm. This may be followed by pitting (deep dents) on the surface of the palm as the diseased tissue pulls on the overlying skin.
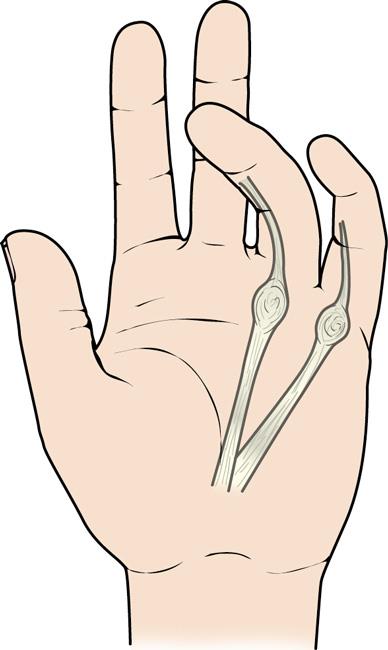
As Dupuytren's gets worse, bands of fascia in the palm develop into thick cords that can tether (lock) one or more fingers and the thumb into a bent position. This is called a "Dupuytren's contracture." Although the cords in the palm may look like tendons, the tendons are not involved in Dupuytren's.
In many cases, a Dupuytren's contracture progresses (gets worse) very slowly, over a period of years, and may remain mild enough that no treatment is needed. In moderate or severe cases, however, the condition makes it difficult to straighten the involved digits. When this happens, treatment may be needed to help reduce the contracture and improve motion in the affected fingers. Typically, as a contracture worsens, the involvement of the fascia becomes more severe, and treatment is less likely to result in a complete correction.
Cause
The cause of Dupuytren's disease is not completely known, but most evidence points toward genetics as having the most important role.
There are anecdotal reports (based on personal accounts) of Dupuytren's developing or worsening after a person experiences an injury or an open wound (including surgery) to their hand; however, there is no good evidence to support this. There is also no convincing evidence to suggest that it is caused by overuse of the hand.
Risk Factors
There are many factors that are believed to contribute to the development or worsening of Dupuytren's disease. These include:
- Gender. Biologic men are more likely to develop the condition than biologic women.
- Ancestry. People of northern European (English, Irish, Scottish, French, and Dutch) and Scandinavian (Swedish, Norwegian, and Finnish) ancestry are more likely to develop the condition.
- Heredity. Dupuytren's often runs in families.
- Alcohol use. Drinking alcohol may be associated with Dupuytren's.
- Certain medical conditions. People with diabetes and seizure disorders are more likely to have Dupuytren's.
- Age. The incidence of the condition increases with age.
- Trauma. Dupuytren's disease may appear and/or worsen after trauma — including surgery — to the hand.
Symptoms
A Dupuytren's contracture typically progresses (gets worse) very slowly, over a period of years. Signs and symptoms of the condition may include:
Nodules. You may develop one or more small lumps, or nodules, in the palm of your hand. These nodules are typically fixed to the overlying skin. Initially, the nodules may feel tender. Over time, this tenderness usually goes away. In some cases, there can be "pitting," or deep dents, in the skin near the nodules.
Cords. The nodules may thicken and contract, contributing to the formation of dense and tough cords of tissue under the skin. These cords can limit or prevent the fingers and thumb from straightening or from spreading apart.
Contractures. As the tissue under the skin tightens, one or more of your fingers may be pulled toward your palm, and you may have trouble spreading them apart. The ring and little (pinky) fingers are most commonly affected, but any or all of the fingers and thumb can be involved.
When a finger is involved in a Dupuytren’s contracture:
- The metacarpophalangeal (MCP) joint is the most common joint to be affected. This is the joint where the finger meets the hand (knuckle).
- The next most common joint to be affected is the proximal interphalangeal (PIP) joint. This is the next joint in the middle of the finger after the MCP joint. Contractures of the PIP joint are harder to treat and less likely to completely recover after treatment than contractures of the MCP joint.
- The distal interphalangeal (DIP) joint, the last joint of the fingers (closest to the fingernail). is less likely than the PIP and MCP joints to be affected by Dupuytren’s disease.
Dupuytren's disease can be progressive, meaning it gets worse over time. As the bend in your finger increases, it may be hard to straighten it fully. It may be difficult to grasp large objects, put your hand in your pocket, or perform other simple activities.
Some patients with Dupuytren's disease may develop thickened tissue on the feet (Ledderhose disease) or penis (Peyronie's disease). Symptoms do not typically occur anywhere else on the body.
Doctor Examination
Your doctor will likely talk with you about your general health and medical history and ask about your symptoms. Because Dupuytren's can run in families, your doctor may ask if you are aware of any relatives who have the disease.
Your doctor will then examine your fingers and hand. During the exam, they will likely:
- Record the location of nodules and cords on your palm
- Measure the range of motion of your fingers and thumb
- Test the feeling in your fingers and thumb
- In some cases, document the appearance of your hand with clinical photographs
These measurements may be compared with other measurements taken throughout your treatment to determine whether the condition is progressing (getting worse) over time.
Treatment
Currently, there is no cure for Dupuytren's; however, the condition is not life- or limb-threatening. Dupuytren's is not a malignancy (cancer) and does not spread to the heart, lungs, brain, etc.
Although its effects vary from patient to patient, Dupuytren's usually progresses (gets worse) very slowly and may not become troublesome for many years. In fact, for some patients, the condition may never progress beyond developing lumps in the palm.
If the condition does progress, your doctor may first recommend nonsurgical treatment to help slow the disease.
Nonsurgical Treatment
Steroid injection. Corticosteroids are powerful anti-inflammatory medications that can be injected into a painful nodule to help reduce symptoms. The effectiveness of a steroid injection varies from patient to patient. While corticosteroids may help with symptoms, they are not likely to keep the disease from getting worse; therefore, they are a treatment, not a cure.
Splinting. While many patients ask about splints to prevent progression of Dupuytren's, splinting is not known to prevent the progression of a finger contracture. Forceful stretching of the contracted finger is not helpful and, in fact, could cause an injury to the finger or hand.
Splinting may be used after surgery for Dupuytren's contracture to protect the surgical site; however, it is not known if wearing a splint reduces the risk of recurrent (repeated) contracture or tightening of the healing wound.
Collagenase injection. The collagen (a type of protein) that makes up a Dupuytren's cord is different than the collagen that makes up the other structures of the hand (e.g. tendons, nerves, blood vessels, and bones). An injectable medication has been developed to take advantage of these differences.
Collagenases are enzymes that break down collagen, and a targeted collagenase was created to specifically break down the collagen in Dupuytren's cords without damaging the collagen of the other important structures of the hand. When injected properly into a Dupuytren's cord, this collagenase can help rupture the cord, allowing for improved motion of the digit (finger or thumb). While the collagenase does not completely remove the cord, symptoms can still be improved following treatment.
Collagenase treatment of Dupuytren's is a two-step process.
- First, the cord is injected with the medication. The medication is then allowed to work for 2 to 3 days.
- Then, at a separate visit, the finger is manipulated (moved in a controlled way by the doctor) until the cord ruptures.
While this is a good non-operative alternative to surgery, it should be noted that recurrence (return) of the disease is higher with this treatment than with surgery. Collagenase injection typically results in less pain and swelling than major surgery and may be a good option in patients with multiple medical issues who are not good candidates for surgery.
Although rare, the injection may cause an allergic reaction or flexor tendon rupture. Other potential complications are the same as those for surgery: infection, nerve or blood vessel injury, pain, and stiffness.
Needle aponeurotomy. Needle aponeurotomy can often be performed in the office with local anesthesia (injection of a numbing medication).
In this procedure, the Dupuytren’s cord is broken up with a small needle that is placed into the cord and then moved precisely until it cuts completely through the cord. While this doesn't remove the cord, putting a break in the cord allows for improved finger motion. As with collagenase injection, recurrence (return) of the disease may be more likely with this treatment than with surgery.
The complications of needle aponeurotomy are rare but may include infection, nerve or blood vessel injury, pain, and stiffness.
Surgical Treatment
If the contracture interferes with hand function, your doctor may recommend surgical treatment. The goal of surgery is to reduce the contracture and improve motion in the affected fingers.
There is no known cure for Dupuytren's contracture; however, surgery is intended to "set back the clock" by reducing the restricting (limiting) effect of the cords by either disrupting or removing them. Unfortunately, the healing tissues will form with the same potential to develop cords in the future — but the gains in hand function can still be significant.
The surgical procedures most commonly performed for Dupuytren's contracture are:
- Fasciotomy
- Partial palmar fasciectomy
Your doctor will talk with you about which procedure is best in your case.
Fasciotomy. In this procedure, your doctor will make an incision in your palm, then divide the thickened cord(s) of tissue. Although the cord itself is not removed, dividing it helps to decrease the contracture and increase movement of the affected finger.
Fasciotomy is typically performed using a local anesthetic that numbs just your hand without putting you to sleep. After the procedure, your wound is often left open and allowed to heal gradually. You will typically have to wear a splint during your recovery.
Because the diseased tissue is not removed, recurrence (return) of the contracture may be more likely for this procedure than for partial palmar fasciectomy (described below).
Partial palmar fasciectomy. In this procedure, your doctor will make an incision, then remove as much of the abnormal tissue and cord(s) as possible to straighten your finger(s). Several types of incisions can be used in a fasciectomy; however, "zig-zag" incisions are typically used. These incisions allow the skin to heal without causing more contracture.
In some cases, your wound will be left open to heal gradually on its own after fasciectomy. In other cases, a skin graft will be needed to help the wound heal. For the skin graft, your doctor will typically take healthy skin from another area of your body and use it to seal the wound. You may have to wear a splint during your recovery.
Partial palmar fasciectomy is a more extensive (bigger) procedure than fasciotomy. It generally means more wound care and physical therapy, a longer healing time, and greater patient effort during recovery. However, the benefit is removal of as much of the diseased tissue as possible, which can help prevent recurrence (return) of the disease.
Of note, in some very severe cases, your doctor may recommend applying a Digit Widget® to the affected finger before surgery. This device, which is typically applied in an operating room, gradually stretches out the finger and cord(s) over about 6 weeks, which can make the Dupuytren's surgery easier to perform, safer, and, potentially, more effective. The device can be removed at the time of the partial palmar fasciectomy.
Complications. As with any surgery, there are risks associated with surgery for Dupuytren's contracture. The likelihood of complications increases with the following:
- The severity of the contracture
- The number of contractures addressed in a single procedure
- The presence of any other medical conditions
Your doctor will discuss each of the risks with you and will take specific steps to help avoid potential complications. Possible risks and complications of surgery for Dupuytren's include:
- Pain
- Scarring
- Injury to nerves and/or blood vessels
- Wound infection
- Stiffness
- Loss of sensation; temporary loss of sensation may result from stretching nerves that have been contracted for a long time
- Loss of viability (ability to live) of a finger/loss of a finger (rare)
Recovery. Severe problems are not common after surgery, but you should expect some pain, swelling, and stiffness. Although the goal of surgery is to improve the ability to straighten the digits, sometimes patients can lose the ability to bend the involved digits due to stiffness. Elevating your hand above your heart and gently moving your fingers will help decrease swelling and should improve stiffness.
Physical therapy can help improve strength and function in your fingers and hand, reduce swelling, and aid in wound care. Often, a hand therapist will make a splint for you to wear during recovery.
Outcomes. Most patients have improved movement in their fingers after surgery. However, because the condition is not "cured" with surgery, about 20% of patients will experience a meaningful degree of contracture recurrence (the contracture comes back). Additional surgery may be required for some patients.
Summary
In general, treatment of Dupuytren's disease can be quite successful. While many patients do not have 100% return to pre-disease motion of their digits, symptoms are often greatly improved following treatment, allowing for return to good hand function.
A very important note is that as Dupuytren's progresses (worsens), it becomes harder to treat and outcomes worsen. Therefore, if you have Dupuytren's or are concerned you may have Dupuytren's, it is a good idea to see a hand surgeon sooner rather than later to ensure the best possible outcome.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.